Lupus in cats: symptoms, diagnosis, treatment
Lupus erythematosus is a cat disease of an autoimmune nature that is truly rare.
Only an experienced veterinarian can make such a diagnosis, and it is necessary to exclude many other diseases that manifest themselves in a similar way. Lupus has a variety of symptoms as the body begins to destroy its own tissue in various organs. Skin lesions are pronounced and characteristic, which is how the disease got its name.
There is no single theory about the causes of systemic lupus erythematosus. Reputable studies indicate a genetic predisposition to the disease, but it manifests itself under the influence of aggressive external factors:
- use of medications;
- ultraviolet irradiation (sun);
- hormonal substances;
- viral infections.
In fact, any problem that disrupts the immune system can trigger lupus. However, it is not clear why, under equal conditions, it is this cat and not another cat that gets sick. There is no age or gender predisposition.
Breed predisposition was identified:
In lupus, special cells responsible for immunity produce antibodies against various tissues of the body's own. Antibodies are a command for destruction. Skin lesions in lupus are the result of the formation of autoantibodies to antigens of epidermal cells.
Causes
The nature of autoimmune diseases in cats has not yet been sufficiently studied. With pemphigus, disturbances in the animal's immune system lead to an attack on the animal's own epidermal cells. The destruction of skin cells and the release of their contents is clinically manifested by the formation of blisters.
- Pemphigus can occur due to the use of drugs as a rare side effect (for example, cephalosporins, ampicillin). In this case, it goes away after discontinuation of the provoking drug.
- The erythematous form can cause.
- Various chronic diseases can also lead to pemphigus due to malfunctions of the immune system. Malignant lymphoma, sarcoma, thymoma, or leukemia may present as pemphigus.
In diseased animals, no relationship with sex, age, or age can be detected.
Picture of the disease
Skin lesions do not always occur, but in approximately every fifth sick animal (in 20% of cases of systemic lupus erythematosus):
- redness and peeling of the entire skin, seborrhea;
- enlarged lymph nodes;
- severe inflammation of the skin around the claws;
- patches of alopecia (baldness) with red, crusty skin, especially around the head and ears.
Systemic manifestations are very serious and can lead to death:
- rapid loss of body weight, exhaustion;
- temperature increase;
- neurological disorders;
- mouth ulcers;
- inflammation of the kidneys (glomerulonephritis);
- inflammation of all joints (polyarthritis);
- progressive muscle weakness and atrophy.
Laboratory tests confirm anemia (outwardly manifested by pallor and yellowness of the visible mucous membranes and weakness). Anemia in such patients is caused by massive destruction of red blood cells. In addition to anemia, hematological analysis may show: leukopenia and thrombocytopenia, which indicates bone marrow damage.
In a urine test, hidden or obvious blood and protein are detected.
Discoid lupus erythematosus
This is a cutaneous form of the disease that is not accompanied by systemic disorders and is therefore not life-threatening. This hypersensitive reaction of the body can be triggered by exposure to ultraviolet radiation on the skin.
A pet should not be diagnosed based solely on external signs; discoid lupus erythematosus in cats has only been diagnosed a few times worldwide.
- lesions are on the face and ears;
- redness, peeling of the skin, crusting;
- ulceration of the skin in the area of the claw bed;
- occasionally – damage to the nasal cavity;
- itching (moderate to severe).
Diagnostics
The final diagnosis is made on the basis of a skin biopsy (a picture of deep dermatitis) and after excluding all other possible diseases:
In case of systemic lupus, a serological blood test is performed: an antinuclear antibody test gives a positive result. To recognize general disorders - damage to the hematopoietic system, kidneys, joints, many other studies may be needed: clinical and biochemical blood tests, ultrasound, x-rays.
Sick animals are also tested for infectious peritonitis, leukemia and feline immunodeficiency viruses.
How successful the treatment will be depends not so much on the doctor, but on the prevalence of systemic lesions. As with other autoimmune diseases of cats, Prednisolone is prescribed in combination with Chlorambucil or other steroid hormones (Dexamethasone, Triamcinolone).
- Prednisolone: 4-8 mg/kg 1 time per day;
- Chlorambucil 0.1-0.2 mg/kg every 24-48 hours.
If the lesions disappear or decrease (usually it takes 1-2 months), the dosage of drugs begins to be gradually reduced. Ideally, remission is maintained with a minimal amount of medication given every other day.
If there is no response to treatment, immunosuppressive drugs other than steroids (Ciclosporine) are tried.
In the case of the cutaneous form (discoid lupus), the animal must be protected from exposure to sunlight. Prednisolone is prescribed in a dose of 2.2 to 4.4 mg/kg daily. Local remedies (ointments) are rarely prescribed.
Treatment is inevitably accompanied by unwanted side effects of steroid hormones. It may be necessary to protect the gastrointestinal tract from ulcerative inflammation and antibiotic therapy in case of secondary infections. To prevent inflammation of the urinary tract, uroantiseptics are constantly used.
Treatment options
This is a disease that has not been fully studied and is quite rare in cats. It cannot be treated with herbs and homeopathic medicines. Veterinarians prescribe steroid hormones and immunosuppressants. There are many drugs of this type and their analogues, but most often they are prescribed:
Vraz describes the exact dosage of the drug for cats. If lupus is effectively treated, the dose is gradually reduced. It takes several months for the owner to notice positive changes in the animal’s condition. When remission is achieved, the amount of medications given to the pet is reduced to a minimum. It is important to know that hormonal medications have serious side effects. Additional gastrointestinal protection or antibiotics may be needed. And in order to avoid the occurrence of inflammation of the genitourinary system, cats are prescribed uroantiseptics as preventive measures.
Autoimmune dermatoses in dogs and cats
Autoimmune diseases
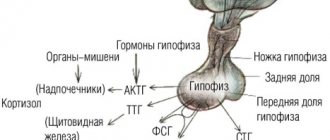
– a group of diseases that are characterized by an excessive reaction of the immune system to the body’s own cells and tissues, the so-called target cells.
Dermatoses diseases
of the pemphigoid complex (pemphigus foliaceus,
pemphigus vulgaris
, bullous pemphigoid, pemphigus vegetans and erythematous), systemic
lupus erythematosus
, discoid lupus erythematosus, auricular polychondritis, vasculitis, cold agglutinin disease,
vitiligo
.
In this disease, the target cells are the intercellular substance in the epidermis
.
As a result, a split occurs between the papillary and stratum corneum. Externally, this process is manifested by the formation of pustules
.
Pustules are usually localized in the area of the muzzle and ears, large in size, symmetrically located. In the absence of pustules, an incorrect diagnosis of allergic dermatitis
.
Systemic reactions may occur - anorexia, fever, apathy. The diagnosis is confirmed with a skin biopsy
.
In this disease, the splitting occurs mainly between the basal and stratum corneum of the epidermis. Clinically, pemphigus vulgaris manifests itself as vesicles and ulcerations on the oral mucosa and mucocutaneous border. Since pemphigus vulgaris occurs with the appearance of ulcers in the oral cavity
, the disease is often severe and can threaten the life of the animal. If pemphigus vulgaris is suspected, calicivirus in cats and ulcerative gingivitis should be excluded. The diagnosis is made based on histological examination of the skin. This disease is characterized by the presence of plasma cells on the basement membrane, which are located in the form of “gravestones”.
Occurs in dogs; this disease is not typical for cats. It is manifested by the appearance of short-term blisters with purulent contents, then they ulcerate. Lesions are localized on the muzzle, mucocutaneous border, abdomen, groin area, and limbs. The analysis is based on a biopsy of the lesions.
It is extremely rare. It appears in a milder form than other forms of pemphigus (multiple papules and pustules). It is important to exclude skin neoplasms. Diagnosis includes histological examination of the skin.
It is considered a mild form of pemphigus. Often the lesions are localized only in the nose area. There is depigmentation of the nose, crusts, ulcers, blisters on the back of the nose and in the bridge of the nose.
For all types of pemphigus, Nikolsky's sign can be positive. Externally it manifests itself as desquamation of the epithelium at the slightest touch. This is due to the fact that the epidermis delaminates and the connection between the layers is disrupted.
Etiology and pathogenesis
The etiology of SLE includes factors related to genetics, environment, and infection, but the exact cause of the disease remains unknown (GrindemandJohnson, 1982). The pathological factors underlying SLE are associated with the presence of high concentrations of antigen antibody complexes in the circulatory system (type III hypersensitivity) or antibodies secreted to a self-antigen on cells such as red blood cells, platelets and leukocytes (type II hypersensitivity; Halliwell and Gorman, 1989). When cell-mediated activity is directed against a self-antigen, type IV hypersensitivity occurs to a lesser extent. Inflammatory lesions caused by antigen-antibody complexes in the circulatory system are not specific to organ systems, but can lead to diseases such as vasculitis, glomerulonephritis, polyarthritis and dermatitis. Soluble immune complexes distribute in the vascular endothelium and cause complement-mediated perivascular inflammation. Inflammatory mediators induce chemotaxis and increase vascular permeability, which may contribute to acute necrotizing vasculitis, fibrinoid deposits, and sclerosis. Immune complex deposits in the kidney cause membranous glomerulonephritis. When immune complexes spread into the synovial membrane, polyarthritis occurs. In pets, as in humans, abnormal immune activation and loss of autotolerance are probably the main causes of the development of SLE. Immune activation can be caused by endogenous (genetic, hormonal, metabolic) or exogenous factors (drugs, ultraviolet radiation, food, infectious organisms such as viruses, bacteria and parasites). Loss of self-tolerance and expansion of the autoreactive B cell population leads to the emergence of autoantibody-producing cells and memory B cells, which may be responsible for periodic outbreaks of the disease.
What it is?
Lupus is the name given to a rare autoimmune disease in cats characterized by the formation of antibodies against the body's own tissues. Let us immediately note that the causes of the disease have not yet been identified. Currently, veterinarians believe that this pathology is genetically determined, since no one has yet proposed more likely predisposing factors.
Lupus is considered a rare disease. But perhaps this opinion is due only to the difficulties of identifying it. It may be that this pathology is much more common. The disease is incurable. Persians, Siamese and Himalayan cats are considered predisposed breeds. The goal of treatment is not a complete recovery, since this is simply physically impossible, but to neutralize the negative impact of the pathological process on the cat’s body. Since the course of the disease inevitably becomes more complicated over time, therapy is indicated in any case.
Predisposing factors
What causes the disease and what are its causes? Alas, we can’t talk about this with confidence, since they have been studied extremely poorly. In general, as is the case with any other autoimmune pathology.
In many cases, we have to admit that all types of disease have an idiopathic etiology. Simply put, the disease appears on one “wonderful” day, and nothing precedes its appearance at all. An assumption may immediately arise that the real reason is lost somewhere in the jungle of genetics and heredity. In addition, there is evidence that the development of the disease is promoted by excessive insolation (UV irradiation from the sun).
What are the signs of damage?
There are two types of lupus that affect cats: discoid lupus (DLE) and systemic feline lupus erythematosus (SLE). The latter is the most serious, since with it the immune system of the animal’s body immediately “goes crazy” and begins to attack almost all tissues and organs. If your cat has been given this particular diagnosis, the prognosis is disappointing. In cats, the main symptom of this disease is gradually developing lameness. Sometimes animals can suddenly fall into a coma. But more often the pathology is accompanied by anorexia and skin lesions (especially in areas regularly exposed to sunlight).
But still, the most typical sign is lameness. Moreover, it often appears suddenly, the joints quickly swell and significantly increase in volume. Other signs may include: periodic fever, various oral ulcers, chronic arthritis (which makes sense), pale gums, hair loss, polyuria and polydipsia, and many neurological pathologies. The diagnosis is made only on the basis of numerous and varied clinical studies.
Therapeutic techniques
In most cases, treatment for lupus in cats consists of prescribing “killer” doses of corticosteroids, which are necessary to “calm down” the immune system. The problem is that long-term use of these drugs will certainly lead to numerous side effects.
It is also recommended to let your cat go outside less often so that he is exposed to the sun's ultraviolet radiation for as little time as possible. In combination with steroids, this approach often achieves stable remission, but, as a rule, it is still followed by a relapse, which in most cases is fatal.
In general, the signs of this disease always depend on which particular system of organs and tissues is “under attack” by its own defense system. Accordingly, treatment is aimed at minimizing the negative manifestations of the disease. So, if a cat suffers from severe joint pain, he is prescribed painkillers and the same corticosteroids, which can somewhat alleviate the inflammatory process. In cases where the pathology affects the nervous system, sedatives and sedatives are prescribed, etc.
Diagnosis of the disease
Diagnosis requires careful analysis and exclusion of many other diseases. Among them, veterinarians identify diseases such as:
- superficial pyoderma;
- dermatophytosis;
- some other diseases of the autoimmune spectrum;
- subcorneal pustular dermatosis;
- eosinophilic pustulosis;
- drug dermatosis;
- dermatomyositis;
- zinc-sensitive dermatosis;
- cutaneous epitheliotropic lymphoma;
- hepatocutaneous syndrome;
- hypersensitivity to insect bites.
Only after all of the above diagnoses have been ruled out can the doctor determine that the problem is pemphigus. The difficulty in determining the disease lies in the fact that in most cases the etiology of the disease is unclear. To confirm the diagnosis, it is necessary to undergo certain tests, among which the following types of examinations are distinguished:
- It is necessary to conduct a cytological analysis of the pustule. Neutrophils and acantholytic cells will be visible in it. Sometimes a laboratory technician can detect eosinophils in the preparation.
- You need to test for antinuclear antibodies. For pemphigus, it should give a negative result.
- But the problem often lies in the unreliability of the data obtained. If you carry out only this type of examination, you can get a false positive result, which will make it difficult to determine the real disease.
- Dermatohistopathology should be performed. It can confirm cytological analysis by detecting subcorneal pustules containing neutrophils with varying numbers of eosinophils.
- The disease can be confirmed by taking a biopsy of the affected skin. The dog's body specimen is sent for immunofluorescence or immunohistochemistry. Its characteristic feature is the intercellular deposition of antibodies. It should be understood that false positive and false negative results are common.
In the event of a secondary infection, it is worth conducting an analysis to detect a bacterial culture in the pustule. If the result is sterile, then the dog has only one disease; if any pathogen is detected, then treatment will be difficult, since two problems will need to be dealt with. The above diagnostic methods allow us to establish a diagnosis.
Discoid lupus
This type of disease can be considered a “benign” variety of the pathology described above. As a rule, the symptoms of lupus in cats are limited to the formation of red spots, predominantly disc-shaped (hence the name), and most often the area of the muzzle or the entire head is affected. You can see these lesions at.
As in the previous case, the animals are prescribed a course of corticosteroids, which help cope with the signs of the inflammatory process. Concomitant administration of broad-spectrum antibiotics is highly recommended. They are also useful for relieving symptoms of inflammation, but more importantly, they can prevent (or treat) secondary bacterial infections. With lupus they often develop.
Symptoms
Symptoms of pemphigus in a dog largely depend on the type of disease. There are four in total:
- Common (vulgaris).
- Erythematous.
- Leaf-shaped.
- Vegetative. The latter type affects dogs exclusively (but extremely rarely).
So, by the presence of what signs can one judge the presence of the disease? Numerous ulcers, pustules and vesicles filled with cloudy contents appear on the surface of the skin. The paw pads are also affected and become prone to cracking and inflammation (the photo shows just such a case).
If the disease is severe, it is accompanied by inflammation and swelling of the lymph nodes, the animal is depressed, and cases of intermittent fever cannot be ruled out. In cases where the paw pads are affected, the animal limps severely, trying not to move at all unless absolutely necessary. All this is accompanied by severe pain and itching.
All types of pemphigus are also dangerous because the sick dog’s body becomes especially susceptible to all secondary bacterial infections. Given the general weakness of the animal, one should not be surprised at the increased likelihood of sepsis.
Pemphigus vulgaris, that is, ordinary, is especially difficult. This type of disease is characterized by the formation of deep and very painful ulcers, “massive” ulcers and pustules. Since they often occur on the mucous membrane of the oral cavity, the animal cannot drink and eat normally. Almost always, pemphigus vulgaris is accompanied by the development of a secondary bacterial infection and fever, and there is a high probability of sepsis. Pemphigus vegetans occurs most easily.
SYSTEMIC LUPUS ERYTHEMATOSUS IN DOGS AND CATS
Peculiarities
Systemic lupus erythematosus in dogs and cats is a multisystem immune-mediated disease characterized by the production of various autoantibodies (eg, ANA, rheumatoid factor, anti-red blood cell antibodies) that form circulating immune complexes. It is rare in cats and uncommon in dogs. Collies, Scottish Shepherds and German Shepherds are predisposed.
Dogs Symptoms are often nonspecific and may wax and wane. Symptoms of skin lesions are common, variable, and often similar to those seen in other skin diseases. Erosion of mucous or mucocutaneous junctions may be observed. Skin lesions may include erosions, ulcers, desquamation, erythema, alopecia, crusting, and scarring of the skin. Lesions may be multifocal or diffuse. They can occur throughout the body, but the muzzle, ears, and distal limbs are most commonly affected. Peripheral lymphadenomegaly is often present.
Other symptoms may include intermittent fever, polyarthritis, polymyositis, renal failure, blood cell abnormalities, pleurisy, pneumonia, pericarditis or myocarditis, central or peripheral neuropathy, and lymphedema. Lesions of the nasal planum, ears and fingertips are unique and characteristic of an autoimmune skin disease. Vesicular cutaneous lupus erythematosus, formerly known as ulcerative dermatosis of shelties and rough collies (UDSSC), appears to be a vesicular variant of cutaneous lupus erythematosus. It is uncommon in shelties and long-haired collies and their crosses. It is typically seen in adult dogs and lesions usually first appear during the summer months. Some dogs may go into remission during the winter and then relapse in early summer. The primary lesions are vesicles and bullae. However, these lesions are often difficult to find because they are fragile and easily ruptured.
Secondary lesions include round, polycyclic and crescent-shaped ulcerations. These lesions typically occur on poorly haired skin (eg, groin, axilla, ventral abdomen, medial thighs) and may progress to involve mucocutaneous junctions, concave auricles, oral cavity, and finger pads. Affected dogs may become weakened and develop sepsis due to a secondary bacterial skin infection.
Cats Skin lesions are variable and may include dermatosis with erythema, alopecia, desquamation, crusting, and scarring; exfoliative erythroderma and excessive peeling (seborrhea). Lesions can be observed throughout the body, but are most often found on the face, ears and paws. There may be mouth ulcers. Other symptoms may include fever, polyarthritis, renal failure, neurological or behavioral abnormalities, hematological abnormalities and myopathy.
Differential Diagnoses Differential diagnoses include other causes of multisystem disease, such as drug reaction, rickettsia and other infections (viral, bacterial, fungal), neoplasia and other autoimmune and immune-related skin diseases.
Diagnosis 1 It is often difficult to make a definitive diagnosis. All differential diagnoses must be excluded. The following findings support the diagnosis and when several findings supporting the diagnosis are found simultaneously (clusters of symptoms), then the diagnosis of systemic lupus erythematosus is highly likely: Hemogram anemia (Coomb test may be positive or negative), thrombocytopenia, leukopenia or leukocytosis. Urinalysis: proteinuria. Arthrocentesis (polyarthritis) sterile purulent inflammation (rheumatoid factor may be positive or negative) ANA test: a good screening test since most patients with systemic lupus erythematosus have positive ANA titers. However, a positive result is only supportive of the diagnosis and is not pathognomonic for systemic lupus erythematosus, since positive titers can be associated with many other chronic or infectious diseases, such as bartonellosis, ehrlichiosis and leishmaniasis. False negative results may occur (10%). Cell test for lupus: A positive result indicates a high likelihood of the disease, but this test is not a good screening test because false negatives are common. 2 Titers should be examined for the presence of rickettsial infection to exclude tick-borne disease. 3 Dermatohistopathology: Focal thickening of the basement membrane zone, subepidermal vacuolization, hydropic or lichenoid superficial dermatitis, or leukocytoclastic vasculitis are characteristic. However, these changes are not always observed and findings may be nonspecific. 4 Immunofluorescence or immunohistochemistry (skin biopsy specimens): plaque deposits of immunoglobulin or complement in the basement membrane area. These methods are not diagnostic in themselves because false positive results are possible and false negative results are common.
Treatment and Prognosis 1 Symptomatic shampoo therapy may be helpful in removing crusts. 2 Appropriate long-term antibiotic therapy (minimum 4 weeks) should be prescribed for the treatment and prevention of secondary pyoderma in dogs. Dogs that received antibiotics during the induction phase of immunosuppressive therapy have significantly higher survival rates than dogs that were treated with immunosuppressive drugs alone. Antibiotic therapy should be continued until immunosuppressive therapy brings the autoimmune disease under control. 3 The goal of treatment is to control the disease and its symptoms using the safest treatments at the lowest possible doses. Typically, combination therapy (see Table) should be used to provide comprehensive treatment while minimizing the side effects of monotherapy. Depending on the severity of the disease, more or less aggressive treatment methods should be chosen. To achieve remission of the disease, higher doses are used initially and then reduced over 2-3 months to the lowest effective dose. Topical treatment given every 12 hours in the form of a steroid-containing drug or tacrolimus will help reduce the severity of focal inflammation and will reduce the doses of systemic drugs required to control symptoms. During remission, the frequency of use of topical medications should be minimized in order to reduce local side effects. Conservative systemic treatments (see Table) include drugs that reduce inflammation and have few or no side effects. These drugs help reduce the need for more aggressive treatments, such as steroids or chemotherapy. Steroid therapy is one of the most predictable treatments for autoimmune skin disease, but the side effects associated with the high doses required to control symptoms can be severe. Although glucocorticoid therapy alone may be effective in maintaining remission, the doses required may result in unwanted side effects, especially in dogs. For this reason, the use of nonsteroidal immunosuppressive drugs, alone or in combination with glucocorticoids, is usually recommended for long-term maintenance treatment. —Immunosuppressive doses of oral prednisolone or methylprednisolone should be given daily (see Table). Once lesions have resolved (after ≈2–8 weeks), the dose should be tapered gradually over several (8–10) weeks to the lowest possible dose every other day that maintains remission. If significant improvement is not observed within 2 to 4 weeks of starting treatment, a concurrent skin infection should be ruled out and alternative or additional immunosuppressive agents then considered. —Alternative steroids for prednisone - and methylprednisolone - refractory cases include triamcinolone and dexamethasone (see Table). —In cats, treatment with immunosuppressive doses of triamcinolone or dexamethasone is often more effective than therapy with prednisolone or methylprednisolone. Oral triamcinolone or dexamethasone should be given daily until remission is achieved (≈2–8 weeks), and then the dose should be gradually reduced to the lowest possible dose and dosing should be as infrequent as possible to maintain remission. —If unacceptable side effects develop or there is no significant improvement within 2 to 4 weeks after starting treatment, consider the use of an alternative glucocorticoid or nonsteroidal immunosuppressive drug (see Table). Nonsteroidal immunosuppressive drugs that may be effective include cyclosporine (Atopica), oclacitinib (Apoquel), azathioprine (dogs only), chlorambucil, cyclophosphamide, mycophenolate mofetil, and leflunomide (see Table). Positive response observed within 8-12 weeks after start of treatment. When remission is achieved, then gradually try to reduce the dose and frequency of non-steroidal immunosuppressive drug for long-term maintenance treatment. 4 Prognosis is guarded if hemolytic anemia, thrombocytopenia or glomerulonephritis is present. In up to 40% of cases, death occurs within the first year of treatment as a result renal failure, poor response to treatment, drug complications or secondary systemic infection (pneumonia, sepsis). The prognosis is more favorable for animals that respond to glucocorticoid therapy alone. In this case, approximately 50% of patients have a long survival period. Regular clinical monitoring is necessary symptoms, general and biochemical blood tests with treatment adjustments as necessary.
Non-communicable diseases
In cats, these diseases are divided into the following groups:
- reproductive system;
- eye diseases;
- endocrine region;
- cardiovascular diseases;
- digestion;
- skeleton and muscular system;
- circulatory system;
- breath;
- urinary excretion;
- nervous system;
- organs of hearing and balance.
Skin diseases
Veterinarians consider skin diseases to be the most common pathologies in cats.
Flea allergic dermatitis
Fleas repeatedly bite through your cat's skin in different places. At the same time, saliva enters the animal’s body, which causes a strong allergic reaction.
Allergic dermatitis can manifest itself as local redness on the skin, itching and swelling at the site of the bite. In some cases, extensive inflammation develops. The degree of damage depends on the number of bites, the duration of the process, the state of immunity, the age of the animal and other factors.
To diagnose flea allergy dermatitis, your veterinarian will order laboratory tests. Based on the results obtained, the doctor selects treatment in the form of a complex of medications.
Important! With constant prevention and proper hygiene, dermatitis in cats goes away quickly.
Eye diseases
Eye diseases in cats can be classified as follows:
- pathologies caused by damage to other organs;
- injuries;
- eye diseases.
Conjunctivitis
Inflammation of the mucous membranes, which rarely manifests itself as an independent disease. In cats, it often accompanies the course of other diseases. It begins due to infection of the eye by microorganisms or in response to allergic irritants.
Symptoms:
- redness of the eye;
- edema;
- profuse lacrimation;
- fear of light.
Sometimes severe itching occurs, so the cat may rub its eyes with its paws. At the same time, the manifestations of the disease only intensify.
First aid consists of washing the eyes with appropriate solutions (potassium permanganate or furatsilin), and then treatment is prescribed by a specialist. If the disease is caused by some other disease, then it is impossible to get rid of it until the cat undergoes a course of basic treatment.
Ear diseases
The most common hearing disease in cats is otitis media. It comes in two types:
- Otitis externa. The inflammatory process affects the auditory canal and occurs in acute or chronic forms. The cause of the disease is infection, any foreign body, or other pathologies. The cat shakes its head, itches, and may refuse to eat.
- Inflammation of the middle ear. The disease rarely develops on its own; it often accompanies third-party infections. Otitis media causes pain and provokes discharge. If left untreated, otitis media can cause the death of a cat.
Ear hematoma
Under the skin of the ear, blood accumulates in the cavity from injuries, bites and mechanical damage. In some mild cases, a tight bandage and ice may be sufficient. A large area of damage will require veterinary intervention and treatment - suppuration and the onset of infectious processes are possible.
Gastrointestinal diseases in cats, their symptoms and treatment
The cat’s gastrointestinal tract is the first to react to low-quality food, bad water and side diseases. With any symptoms of illness, cats first refuse food or significantly reduce its consumption.
Intestinal obstruction
Blockage of the gastrointestinal tract occurs for various reasons and is expressed in the inability of food mass to pass through the gastrointestinal tract.
Causes of the disease include:
- the presence of a foreign body in the gastrointestinal tract;
- volvulus - twisting of a ligament of lymph nodes and blood vessels;
- intussusception of the site - two segments of the intestine enter one another, while the animal experiences severe pain;
- intestinal parasites;
- neoplasms – lymphoma or lymphosarcoma;
- hairballs that enter the gastrointestinal tract when the cat licks its own fur coat;
- constipation.
Treatment involves improving intestinal motility, intravenous nutritional infusions, antibiotics and other special veterinary measures. Without urgent veterinarian intervention, the disease develops towards death.
Respiratory diseases
This group of diseases often appears against a background of weakened immunity and after complex infections.
- Rhinitis is an acute or chronic inflammatory process of the nasal cavity with swelling of the mucous membrane and difficulty breathing.
- Laryngitis is a lesion of the larynx, which is accompanied by a cough, change in voice and pain.
- Primary or secondary bronchitis.
- Emphysema is an increase in lung volume.
Most often, the disease cannot be eliminated on its own, so the animal owner needs to contact a veterinary clinic so that a specialist can prescribe the correct treatment.
Diseases of the genitourinary system
The main function of the urinary system is to remove waste and unnecessary substances. Therefore, any failures immediately lead to serious problems, provoke new diseases in cats and require immediate treatment from a veterinary specialist.
Idiopathic cystitis in cats, symptoms and treatment
The disease affects the lower urinary tract. Its symptoms are similar to other ailments in this area.
Symptoms:
- painful sensations when urinating or difficulty doing so;
- frequent urge;
- there is blood in the urine;
- The cat constantly licks itself in the genital area.
The disease causes severe pain to the animal and it is impossible not to notice it.
Diagnosis in veterinary clinics is carried out by urine analysis, bacterial cultures, x-rays, and ultrasound. Combined treatment - proper nutrition with plenty of moisture and medications as prescribed by a doctor.
ICD in cats, treatment and prevention
Urolithiasis affects cats of absolutely all breeds - according to statistics, the pathology is diagnosed in every 10 pets. The causes of the development of the disease are most often factors such as:
- metabolic disease;
- lack of nutritional balance;
- genetic predisposition;
- obesity.
The main symptoms of the disease include frequent urination (often past the tray). Urine is excreted in small quantities, sometimes with blood. The process causes severe pain to the animal; the cat makes plaintive sounds and constantly licks its stomach.
In the absence of proper treatment, intoxication of the body begins, the abdomen enlarges, the body temperature decreases and the cat dies after 2-3 days.
As treatment, the veterinarian performs catheterization and prescribes drug therapy.
Pyometra
Purulent inflammation of the uterus most often affects older cats. The disease develops due to bacterial intervention in the period after the end of estrus or due to hormonal drugs that are given to the animal to reduce sexual activity. Pyometra can also be caused by uncontrolled mating and a sedentary lifestyle.
The initial stage of the disease is asymptomatic. Later, the cat's appetite decreases and it loses weight. Hair falls out, and discharge with an unpleasant odor appears from the genitals. Successful treatment involves surgery, removal of the ovaries and uterus. Then drug therapy is prescribed.
Diseases of the cardiovascular system and their symptoms
Another group of common diseases that affect cats of all breeds. Symptoms of cardiovascular pathologies include:
- Cough, shortness of breath, bluish coloration of mucous membranes, pulmonary edema - this is left ventricular failure.
- Fluid in the abdominal cavity and chest, swelling of peripheral organs - stagnation of blood in the systemic circle and right ventricular failure.
- Cardiac arrhythmia - collapse, change in the sequence of heart contractions, uneven pulse.
Diseases of the endocrine system in cats, their symptoms and treatment
The functioning of the endocrine glands most often fails in older cats. At the same time, there is an exacerbation of dermopathy that accompanies endocrine problems.
Hyperthyroidism
The disease is associated with dysfunction of the thyroid gland and increased production of certain types of hormones (thyroid). The gland enlarges and sometimes begins to degenerate. The percentage of malignant changes is small (2%), most often we are talking about a benign process.
Symptoms of the disease:
- metabolism accelerates and appetite increases;
- weight loss;
- muscles atrophy;
- the cat drinks a lot and urinates little;
- Possible vomiting or diarrhea.
Sometimes the animal shows unmotivated aggression and strives for loneliness. These signs are mistakenly attributed to old age and attention is not immediately paid to them.
Diagnosis of hyperthyroidism involves clinical laboratory and instrumental studies.
Treatment may be medication or surgery.
Diabetes mellitus in cats
A common endocrine disease, the exact cause of which has not been identified. Most often, the pathology is diagnosed in overweight animals.
Diabetes mellitus in cats is classified as follows:
- In the first type, it manifests itself regardless of age; in the future, the animal remains in the insulin-dependent group for life.
- The second type is typical for older cats that have normal or increased weight and reduced insulin sensitivity. They can even skip injections without dying.
- The third type is a pathology with damage to the pancreas. Treating the underlying cause will improve the disease, but cats still need insulin.
Important! Excellent prevention of diabetes is a low-fat diet, exercise and mandatory annual examinations by a veterinarian.
Experts believe that all existing cat diseases primarily affect their appetite, activity and coat condition. As soon as your pet’s behavior changes, deviations from its usual rhythm of life are observed, or its appearance deteriorates, it must be urgently shown to a specialist to find out the cause of the changes.