- Etiology of hypertrophic cardiomyopathy in cats
- Symptoms of hypertrophic cardiomyopathy
- Diagnosis of hypertrophic cardiomyopathy
- Treatment of hypertrophic cardiomyopathy
- Prognosis for hypertrophic cardiomyopathy
Feline hypertrophic cardiomyopathy (FCM or HCM) is a very insidious and common disease of cats, which is characterized by thickening of the wall of the left ventricle and the interventricular septum. In this case, a significant decrease in the volume of the left ventricular cavity occurs, which can provoke an enlargement of the left atrium. The myocardium is involved in the process, which leads to disruption of the normal functioning of the heart muscle. According to statistics, this problem most often occurs in males.
Feline heart disease
Pathologies occur both congenital and acquired. All existing diseases are classified according to location and cause of occurrence:
- Heart defects.
- Tissue mutations.
- Disorders of heart rhythm and conduction of electrical impulses.
- Parasitic origin.
- Inflammatory. They develop in organ tissues. The following diseases are distinguished by location:
- pericarditis;
- myocarditis;
- endocarditis.
Among these problems, cardiomyopathy develops most often in cats.
Structure of a cat's heart
GENETIC DISEASES
The most common genetic diseases in cats are: cardiomyopathy (enlargement of the wall of the ventricles of the heart) in American Shorthairs, Maine Coons, Ragdolls, Siamese, and Siberian cats. Hypotrichosis (baldness) often occurs in Abyssinians, Bengals, Himalayans, Siamese Coshes, Cornish and Devon Rex). Bone deformities are also not uncommon in purebred cats, for example, hip dysplasia (in Burmese, Chartreux, Devon Rex, Maine Coons, Persians, Exotics and Siamese) and funnel chest deformity (Munchkins, Maine Coons, Ocicats). Another serious genetic disease that can lead to the death of an animal is polycystic kidney disease . This problem is most often encountered by American Shorthair, Himalayan, Persian and Scottish Fold cats.
Cardiomyopathy: etiology and pathogenesis
Feline hypertrophic cardiomyopathy (HCM) is a pathology accompanied by hardening of the walls of the ventricle. As the disease develops, the volume of the heart chambers is significantly reduced, subsequently provoking heart failure. Timely treatment helps prevent death, but in advanced forms of the disease the prognosis is poor. The disease mainly manifests itself early in the pet's life - at the age of 6 months.
Animals with genetic heart abnormalities do not survive to puberty
HCM is considered a relatively new disease. Research into this pathology was actively carried out at the beginning of the last decade in the USA.
Scientists have concluded that breeds most susceptible to the disease include Ragdoll, Sphynx , Norwegian Forest, Scottish Fold , Persian and Abyssinian breeds. In Maine Coons, transmission of the disease at the genetic level has been confirmed. Most often the disease is observed in males.
The most susceptible breeds to the disease
Among such mass-bred breeds as Siamese , British Shorthair , Siberian and Russian Blue, no hereditary predisposition has been identified. Representatives of these varieties suffer from secondary forms of pathology.
What happens to the heart with HCM?
The clinical picture of a typical cardiomyopathy is characterized by the following manifestations:
- Reduction in the size of the left ventricle, which can lead to a decrease in the amount of blood supplied. In addition, the mobility of the walls decreases. This leads to the release of blood into the vessels of the lungs.
- As the disease progresses, the left atrium enlarges. The resulting blood clots contribute to impaired hemostasis, leading to paralysis of the hind limbs.
- Further, the mitral valve is involved in the pathological process. As a result of a change in its location, an obstruction occurs in the exit of blood into the aorta. This hitch in the blood flow is accompanied by a systolic murmur.
- Myocardial compaction causes blood stagnation in the atria and malfunction of the atrioventricular valve. As a result, aortic obstruction and circulatory deficiency are noted.
Image of a heart affected by pathology
Types of HCM
Hypertrophic cardiomyopathy of furry pets is divided into 2 types: primary and secondary. The origin of the first type, which occurs in obstructive and non-obstructive forms, is currently under study. The second (acquired) develops under the influence of another disease.
Table 1. Types of HCM in cats
| Type | Characteristic |
| Obstructive | Due to the expansion of the myocardium, the pressure in the left ventricle increases, which increases the rate of blood flow into the aorta. As a result, the bicuspid valve leaf opens and closes involuntarily |
| Non-obstructive | The mechanism of manifestation of the pathology is identical to the previous one, except that high blood flow speed does not affect the functioning of the valve |
| Acquired | It is provoked by existing diseases and age-related transformations, accompanied by mutations in the structure of the myocardium. Infectious pathologies, disruptions in the endocrine system, injuries and toxins are the triggering factors. |
The primary type of the disease, which is characterized by genetic origin, manifests itself before 5 years. The secondary form occurs mainly in older cats after 7 years.
The secondary form of the disease occurs in adult cats
Possible complications
The progression of hypertrophic cardiomyopathy affects all parts of the heart and the circulatory system as a whole. This occurs due to the overcrowding of the lung vessels with blood. Due to slow blood circulation in the cat's heart chambers, blood clots form.
The danger of HCM is the formation of blood clots
How does a coma manifest?
Symptoms in a cat of coma caused by kidney failure, liver failure, or diabetes mellitus always have characteristic features.
The animal falls into a lethargic state for several days, and body temperature decreases. The cat stops responding to external stimuli - noise, screams, and respiratory activity becomes very weak.
A characteristic difference between a comatose state in a cat and death is the absence of rigor mortis.
Most often, diabetic coma is diagnosed in cats, which develops quite slowly, because from the onset of the pathological process to the complete loss of consciousness by the animal, it takes from several days to one week.
There are several characteristic periods of hyperglycemic coma:
- Precomatose - characterized by increased thirst and urine output, a sharp decrease in total body weight, nausea and eruption of gastric contents. There is general weakness in the cat, itching on the skin, an increase in ketone bodies in the general analysis, and then passes into the stage of incipient coma.
- An incipient coma is characterized by increased vomiting with blood clots, increased thirst, the appearance of a strong smell of acetone from the mouth, painful sensations in the abdominal area, and dehydration.
- Coma is the final stage, which is characterized by the presence of dry skin, softening of the eyeballs, and a decrease in body temperature to critical levels. If the temperature rises, one should suspect the presence of an associated infection. The breathing of a sick animal changes, a dark brown coating is detected on the tongue, the muscles are relaxed, the pulse is rapid and incomplete.
In addition, signs of the onset of coma in a cat are:
- A sharp decrease in pressure in the arteries. This is primarily due to disturbances in the functioning of the myocardium, atrial fibrillation, as well as extrasystole of the ventricular type;
- Increased excretion of urine with an increased content of ketone bodies, proteins and glucose, and upon microscopic examination, red blood cells and casts are noted in the urine.
- Changes in blood test - there is an increased content of ketone bodies, protein particles, creatinine and urea. In addition, the erythrocyte sedimentation rate increases, and leukocytosis is also noted.
- A change in the level of immunoreactive insulin, accompanied by dehydration, loss of electrolytes, a decrease in sodium particles and an increase in potassium particles. As a consequence, disruption of the sodium-potassium pump leads to disruption of myocyte function.
Symptoms of the disease
The main manifestations of hypertrophic cardiomyopathy are poor exercise tolerance and shortness of breath. If the disease is asymptomatic, there is a high probability of death due to thromboembolism, which develops as a result of pulmonary edema.
Dyspnea and paralysis are common in HCM
The main signs of HCM are the following symptoms:
- Physical state. An exhausted animal loses interest in active games and sleeps a lot.
- Breath. Severe, accompanied by wheezing and gurgling. Under heavy load, the pet experiences difficulty in inhaling. This is caused by slowing down the movement of blood in the veins. The cat breathes with its belly, sticking out its tongue.
- Dyspnea. Attacks of suffocation often lead to fainting as a result of lack of oxygen.
- Character of the pulse. Filiform.
- Condition of mucous membranes. Due to oxygen starvation, the shells acquire a blue tint.
- Cough. Reflex, caused by excessive pressure of an enlarged heart on the trachea. To cope with an attack, the cat sticks out its neck, spreading its forelimbs for greater ventilation.
- Hydrothorax and ascites. The release of exudate contributes to the formation of swelling in the peritoneum and chest.
- Paralysis of the hind limbs. If a blood clot blocks the lumen in the vessels, the animal’s legs in the pelvic area fail.
- Body mass . Poor weight gain.
- Heart murmurs and tachycardia.
If you notice any of the symptoms, take your pet to the veterinarian
Symptoms of hypertrophic cardiomyopathy
The main symptoms of feline hypertrophic cardiomyopathy are:
- Depressed state of the animal;
- Heavy breathing, which is accompanied by wheezing or even “gurgling”;
- Dyspnea;
- Tachycardia;
- The mucous membranes acquire a bluish color;
- Thromboembolism (in most cases one pelvic limb fails, occasionally both);
- Heart murmurs;
- Pulmonary edema;
- Accumulation of fluid in the chest cavity (hydrothorax);
- High blood pressure;
- Fainting.
Cats with heart pathologies do not have a cough!!!
Death can come suddenly!!! Therefore, if at least one of the symptoms appears, you need to contact the nearest veterinary clinic as soon as possible to diagnose the disease and provide the necessary veterinary care.
It is possible that the disease can occur latently, that is, hidden. The animal is not bothered by anything and does not in any way show the fact that changes are already taking place in its body. But any influence from the external environment can provoke the rapid development of this pathology. Mostly it's stress. Infusion therapy (intravenous drip administration of drugs) can also serve as a catalyst if the volumes and speed of infused fluid do not correspond to the parameters of the animal.
Due to increased pressure in the vessels, stagnation occurs, against which pulmonary edema develops. Swelling can lead to fluid accumulation in the pleural cavity. It becomes difficult for the animal to breathe. Breathing becomes heavy, insufficient oxygen enters the body, which can lead to hypoxia.
One may suspect that a cat has developing heart disease after physical exertion or severe stress. The animal lies on its stomach and spreads its paws wide, breathing with an open mouth like a dog. After the animal has rested, its condition may return to normal.
Often occurs several days later or immediately after the use of general anesthesia. If it appears immediately, it is in a severe form.
Reasons for the development of the disease
The main cause of the disease is considered to be a gene mutation. The pathology is inherited among some cat breeds. American experts concluded that the gene responsible for myosin binding protein is to blame. Maine Coons and Ragdolls are predominantly affected by this gene mutation. It has been proven that more than 10 genes are involved in the development of the disease.
Representatives of the Maine Coon breed are more susceptible to pathology than others
In addition to breed predisposition, a number of other reasons influence the development of cardiomyopathy.
Table 2. Provoking factors
| Provoking factor | Characteristic |
| Congenital myocardial pathologies | Any diseases occurring in this part of the heart are fraught with hardening of its walls |
| Infusion therapy | If the rate of intravenous penetration of the drug into the pet’s body does not correspond to its physiology, the pressure in the vessels increases. As a result, stagnation occurs, leading to swelling of the lungs. Insufficient oxygen supply leads to hypoxia |
| Malignant neoplasms | The formation of lymphoma is fraught with mutation of the myocardial structure |
| Endocrine diseases | Increased activity of the thyroid gland contributes to the development of tachycardia. Due to increased production of growth hormone, the walls of the heart muscle thicken |
| Taurine deficiency | This amino acid, essential for cats, regulates organ contractility, has an anti-ischemic effect and maintains the integrity of cell membranes. Deficiency of this element destabilizes the heart muscle |
| Application of anesthesia | Pets may develop hypertrophic cardiomyopathy after being under general anesthesia. The disease manifests itself either immediately or several days after artificial immersion in sleep |
| Chronic intoxication | Overdose of medications, chemical poisoning, products of pathogenic activity of parasites negatively affect the fibers of the heart muscle and contribute to the development of ventricular hypertrophy |
| High blood pressure | Constant deviation from the norm provokes wear and tear of the organ |
Heart disease in cats. Cardiomyopathies. What is HCM and DCM?
Cardiomyopathy – what is it?
Cardiomyopathy is a collective concept that refers to a whole group of heart diseases characterized by dystrophic changes in the myocardium (heart muscle).
Based on the nature of the changes occurring in the heart, several types of cardiomyopathies are distinguished. The main, and most common, include hypertrophic cardiomyopathy (HCM) and dilated cardiomyopathy (DCM) .
HCM is characterized by thickening of the walls (totally or just one area) and a decrease in the cavity of the ventricles of the heart. This is the most common form of cardiomyopathy in cats (about 65% of all cardiomyopathy in cats).
DCM, on the contrary, is characterized by thinning of the walls and dilation of the ventricular cavities. It is relatively rare (about 5%).
It is necessary to say the same about other forms of cardiomyopathy: RCM (restrictive cardiomyopathy, as with HCM, the pathological process affects the left ventricle, but myocardial thickening is less pronounced), ARVD (arrhythmogenic dysplasia of the right ventricle - changes mainly affect the right ventricle), In some cases, transformations in the heart are difficult to unambiguously interpret; such diseases are classified in the group “Unclassified cardiomyopathies.”
Causes of the disease
Depending on the causes of cardiomyopathy, there are:
Primary or idiopathic. This form of the disease is believed to be genetic in nature. Currently, gene mutations have been identified that lead to HCM in the Maine Coon and Ragdoll cat breeds. Several other breeds, including the British Shorthair, American Shorthair, Scottish Fold, Sphynx, Persian, and Norwegian Forest, have a family predisposition to hypertrophic cardiomyopathy. In these breeds, hereditary forms are also assumed, and research in this area is ongoing. It is also believed that cats of the Abyssinian, Thai, Burmese, and Siamese breeds are predisposed to DCM. In rare cases, idiopathic cardiomyopathy is also detected in outbred animals.
Fig.2. Maine Coon cats
Fig.3 British Shorthair
Fig.4 Sphinx
The secondary form of the disease is suspected in cases where there is a disease that is the cause of changes in the myocardium. For example, arterial hypertension, hyperthyroidism, an inflammatory process in the heart muscle - myocarditis, heart defects (aortic stenosis) can lead to secondary myocardial hypertrophy, and DCM can be caused by a lack of taurine due to unbalanced feeding, myocarditis, heart defects.
Fig.5 Burmese cat
Fig.6 Abyssinian cat
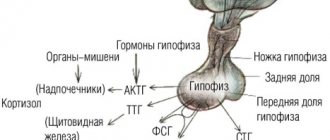
Mechanism of disease occurrence (pathogenesis)
The pathological process can affect various parts of the myocardium, but damage to the left ventricular myocardium is of greatest importance in the manifestation of the disease. With DCM, this is a decrease in the “pumping” function, the inability of the ventricle to adequately contract and push blood into the systemic circulation. And with HCM, on the contrary, this is the inability of the heart muscle to relax, and, as a result, insufficient blood volume entering the systemic circulation. Whatever the reason for the changes, these changes lead to an increase in pressure in the left atrium, and subsequently, an increase in pressure in the pulmonary veins - the vessels through which blood enters the left atrium. Then the pressure in the smaller vessels and capillaries of the lungs increases and, as a result, pulmonary edema, sometimes hydrothorax, develops. These are the most serious manifestations of the disease and can lead to the death of the animal.
Involvement of the “right heart” in the process sometimes causes fluid accumulation in the abdominal cavity (ascites), chest cavity (hydrothorax), and pericardium.
In addition to these obvious symptoms, a whole cascade of adaptive reactions follows, which subsequently lead to irreversible changes, both in the heart itself and in other organs. Such processes include tachycardia (uncontrolled prolonged increase in heart rate), arterial hypertension (increased blood pressure), vasoconstriction (narrowing of blood vessels), thirst (rare in cats).
Clinical picture
In the early stages of the disease, and sometimes even with more pronounced changes in the heart, symptoms may be absent. In some cases, you may notice that the cat has become less mobile; during physical activity, the breathing rate increases. This “hidden” stage can last quite a long time; symptoms begin to increase, as a rule, after some provoking factor: stress, surgery, anesthesia.
The main manifestation of the disease is increased breathing - shortness of breath. If at the beginning of the disease it can manifest itself unnoticed, for a short time, mainly after physical activity, then over time it progresses and appears at rest. With the development of pulmonary edema, the cat takes a forced position, often breathes with an open mouth, you can notice that the tongue and gums acquire a bluish tint. If emergency assistance is not provided in this situation, the animal will die.
Another complication that develops with cardiomyopathies in cats is vascular thromboembolism. A blood clot formed in the dilated chambers of the heart breaks off and begins to migrate through the blood vessels. Manifestations of thromboembolism depend on which vessel the thrombus stops and blocks. The most common location is the femoral arteries. In this case, paresis of the pelvic limbs develops. The cat does not lean on its paws, the pads of the toes are cold, and the pulse on the affected limbs cannot be felt. As a rule, there is severe pain.
In some very rare cases, the only manifestation of the disease may be sudden death.
How to identify?
The “gold standard” in the diagnosis of cardiomyopathies is the echocardiographic method (cardiac ECHO).
For Maine Coon and Ragdoll cats, there are special genetic tests for the presence of mutations that cause HCM (HCM test). But this test does not exclude echocardiography, since the presence of this mutation does not mean the presence of the disease itself. The disease can develop later, in different forms and varying degrees of severity. Changes detected by echocardiography are the basis for starting treatment. Likewise, a “negative” result does not exclude echocardiography. It has been proven that the disease can develop in animals with a “negative” test for HCM; it is assumed that the disease is polygenic in nature (more than 400 gene mutations leading to HCM are known in humans).
Genetic testing of cats is necessary, first of all, for planning breeding work and culling from breeding individuals who are carriers of mutated genes.
In addition to echocardiography, during a cardiac examination, electrocardiography (ECG) may be required to identify complications in the form of heart rhythm disturbances. In addition, in some situations, X-rays, ultrasound of the chest cavity, and laboratory tests are used.
How to treat?
Treatment is aimed at eliminating the symptoms of congestive heart failure and preventing pulmonary edema; for these purposes, diuretics are prescribed. In order to understand the severity of congestion, a test of counting respiratory movements per minute is used. This is a simple way to assess the condition of an animal at home, which even the owner can use. To do this, at rest, count the respiratory movements (that is, each inhalation and exhalation) per minute. Normally, the respiratory rate does not exceed 27 respiratory movements per minute.
For the treatment of chronic heart failure, drugs from the group of ACE inhibitors are prescribed.
When dilated chambers of the heart are detected, prevention of thrombus formation is necessary; for this, as a rule, drugs from the group of antiplatelet agents are prescribed.
To control tachycardia and improve myocardial elasticity (in HCM), β-blockers are sometimes used.
In some situations, drugs that enhance myocardial contractility are needed.
Treatment should be prescribed by a veterinary cardiologist based on the examination of the cat.
How long will a cat live?
Despite the uniform principles and stages of development of the disease, predicting the life expectancy of cats with cardiomyopathy is a rather complex issue. Even the same forms of cardiomyopathy in different animals are individual in nature, so life expectancy and the severity of the disease can vary significantly. This happens because in addition to the reasons that caused the disease, there are a number of external and internal factors (such as stress, concomitant diseases and even the character of the cat) that can influence the course of the disease.
What to do? prevention
Prevention consists of early detection of the disease and competent breeding work. There are no drugs with proven effectiveness in preventing the development of the disease. Therefore, it is very important to detect the disease in a timely manner.
For this purpose, a preventive examination by a cardiologist and echocardiography are recommended in the following groups:
- Cats belonging to risk group breeds* before undergoing surgical interventions under general anesthesia.
- Regularly for animals of risk group breeds* once every 1-1.5 years until they reach the age of five.
- For older cats over 6 years of age, undergo surgery under general anesthesia.
- Animals that demonstrate rapid breathing during light exercise or at rest, increased fatigue during exercise or when a cardiac murmur or arrhythmia is detected during a therapeutic examination.
* Maine Coon, Ragdoll, British Shorthair, American Shorthair, Scottish Fold, Norwegian Forest, Sphynx, Persian, Abyssinian, Thai, Siamese, Burmese
In the network of clinics “Your Doctor” you can conduct a cardiological examination of your animal. You can find out more about the service and make an appointment by calling.
Diagnosis of the disease
The difficulty of detection is caused by the hidden nature of the pathology. Malfunctions in the functioning of the organ can be detected by listening to heart murmurs. In the presence of HCM, they resemble a gallop.
An echocardiogram is considered the most informative way to diagnose HCM
Basic methods:
- Anamnesis collection. The owner must describe the pet's condition in detail. Any deviation in behavior may signal the development of the disease.
- Echocardiography is the most accurate diagnostic method. It makes it possible to thoroughly study the structure of the heart muscle. Each cat that is at risk by breed should be examined at least once a year. Before surgery that involves the use of anesthesia, it is also necessary to check for the presence of HCM.
- Electrocardiography. This survey is not informative enough. It can be used to detect tachycardia, ventricular arrhythmia and widening of the QRS interval. However, it is not used as an independent method for diagnosing pathology.
- X-ray diagnostics. The shape and size of the heart muscle, as well as the presence of fluid in the pleural cavity, are assessed.
- Auscultation. Listening allows you to identify extraneous noise and evaluate your heart rhythm.
- Pressure measurement. With HCM, blood pressure will be elevated.
- Visual assessment. Blue discoloration of the mucous membranes indicates a malfunction of the heart muscle.
Pressure measurement is an auxiliary diagnostic method
If the animal has a severe form of hypertrophic cardiomyopathy, hardware examinations are not performed. Any manipulation negatively affects the emotional state of the pet and increases the manifestation of unpleasant symptoms.
SYMPTOMS OF CAT DISEASE
The following symptoms indicate that your purr is sick:
- Refusal of food and water or, on the contrary, excessive appetite;
- Problems with wool. Severe hair loss, dullness, and the appearance of bald patches – all this indicates an imbalance in the cat’s body. Hairless cats may develop dermatitis, skin sores, or peeling.
- Purulent or cloudy discharge from the eyes, nose, and ears;
- Increased or, conversely, decreased temperature (normally it is in the range of 37.5–39ºC)
- Vomiting or diarrhea;
- Blood in the urine and stool, difficulty urinating.
“A cat is the whole world” is an absolutely true statement. Not only figuratively, but also literally: in the gastrointestinal tract of every cat lives a whole ecosystem of beneficial and pathogenic microorganisms, the “force of good” and the “force of evil.” If a cat is healthy, its “good” always defeats “evil”. And the tray is in complete order. This ecosystem of bacteria, protozoa, viruses and microscopic fungi is called a biome, or microbiome. Hill's Pet Nutrition has spent a decade studying the microbiome of cats.
The result of these studies was a new dietary food for cats, Hill's PRESCRIPTION DIET Gastrointestinal Biome with chicken. The diet contains advanced ActiveBiome+ ingredient technology. This unique blend of prebiotic dietary fiber helps maintain microbiome balance, naturally restoring normal, regular bowel movements in your cat . The diet is rich in Omega-3 and Omega-6 polyunsaturated fatty acids and contains clinically proven antioxidants* that help support a healthy immune system.
Hill's new helps promote healthy digestion in cats, which helps improve overall body health.
When choosing a special food, be sure to consult a veterinarian
Treatment of the disease
The developed treatment regimens for pathology do not make it possible to completely overcome the disease. The main emphasis is on symptomatic therapy. In severe cases, in addition to medication, special equipment is used.
Hospital treatment
The duration of stay in the clinic is 3 days. Any hardware intervention is carried out as carefully as possible in relation to the animal. Basic procedures:
- To stabilize the condition, the animal is placed in an oxygen box, which is a chamber with a constant supply of oxygen.
- After you feel better, if necessary, the fluid accumulated in the pleura is removed (thoracentesis). This helps ease the breathing process.
While in the clinic, owners are allowed to visit their pets. Such visits speed up the healing process.
One of the methods of express therapy is thoracentesis.
Drug treatment
Therapy is based on stabilizing the heart rate, preventing the formation of blood clots and relieving pulmonary edema.
Drugs used:
- Beta blockers. "Verapamil" and "Carvedilol". Reduces the load on the heart.
- Thrombolytics. "Alteplase". Blood clots dissolve.
- Antiplatelet agents. Heparin and Aspirin. Prevents the formation of blood clots.
- Diuretics. "Temisal", "Eufillin" and "Furosemide". Reduce congestion and eliminate swelling.
- Taurine-containing preparations. Thin the blood and improve the condition of blood vessels. Vitamins for cats from, GimP.
Beta blocker "Verapamil" has a positive effect on cardiac tone
For older pets suffering from secondary hypertrophic cardiomyopathy, the root cause is eliminated. Animals must be registered with a veterinarian and undergo regular examinations.
The dosage is prescribed by the doctor, based on the degree of organ damage.
Diet food
In addition to taking medications, the cat is put on a special diet that helps stabilize blood pressure. It is based on avoiding salt. This substance promotes fluid retention.
It is important to enrich the nutrition plan with the following elements:
- taurine;
- fatty acid;
- L-carnitine.
If there is a lack of vitamins, food supplements are given, sold in veterinary pharmacies.
Therapeutic diet involves avoiding salt intake
If before the onset of HCM the diet consisted of dry food, it is necessary to switch the animal to food designed for pets with pathologies of the cardiovascular system.
During treatment, the animal should not be overfed, since obesity contributes to the formation of additional stress on the heart.
Excess weight negatively affects the functioning of the heart muscle
Treatment of cats with DCM
Hypothermia is common in cats with decompensated DCM.
Therefore, if necessary, it is necessary to provide external heat sources to warm the animal. Pleural fluid is removed by thoracentesis. Once pulmonary edema is controlled, diuretics such as furosemide (1 mg/kg - 0.35 ml) are given orally every 12 hours. Diuretics are given to promote diuresis, as previously described for VSMC. The venoditator nitroglycerin may be useful in cats with severe pulmonary edema. Vasodilators (eg, Benazepril tablet 5 mg orally every 24 hours or pimobendan tablet 1.25 mg orally every 12 hours) may help maximize cardiac output, although with the risk of hypotension. Blood pressure, hydration, renal function, electrolyte balance, and peripheral perfusion should be monitored continuously.
Intravenous digoxin was also used initially in cats with decompensated DCM. Amrinone is a positive inotropic agent with peripheral vasodilating properties, although the exact dosage for cats has not been established. Oral digoxin is the positive inotropic drug of choice for maintenance therapy. Digoxin tablets are commonly used because many cats do not like the taste of digoxin syrup. Toxicity can easily occur, especially if other drugs are used concomitantly, so periodic assessment of serum digoxin levels is required.
Furosemide and vasodilators may reduce cardiac congestion and accelerate the development of cardiogenic shock in cats with DCM. Isotonic saline with 5% dextrose in a 1:1 ratio or other low-sodium solutions can be given intravenously at doses of 20-35 ml/kg/day several times a day or by continuous infusion. Potassium supplementation may be required. Fluid can be given subcutaneously if necessary, although absorption of fluids from the extravascular space may be impaired.
Long-term treatment for cats that survive acute heart failure includes the oral medications pimobendan, furosemide, an ACE inhibitor, digoxin, aspirin (or warfarin), and a taurine supplement or high-taurine diet. Taurine supplementation, 250–500 mg orally every 12 hours, should be administered as soon as possible in cats with low or normal plasma taurine concentrations. Taurine is available in 500 mg capsules from sports and health food stores. Since clinical improvement usually does not begin after 1 to 2 weeks of taurine supplementation, maintaining cardiac treatment is vital. Treatment with aspirin or warfarin is usually used to reduce the risk of thromboembolism. Echocardiographic evidence of improved systolic function is observed in most cats within 6 weeks of starting taurine. Drug therapy may become unnecessary in some cats after 6 to 12 weeks, although it is recommended that resolution of pleural effusion and pulmonary edema be confirmed radiographically before stopping the cat's medication. When echocardiographic measures of systolic function are at or near normal, the amount of taurine may be reduced and therapy eventually discontinued as long as the cat eats a diet known to maintain adequate plasma taurine concentrations (eg, most good commercial diets). ). Dry diets with 1000 to 1200 mg taurine per kilogram dry weight and canned diets with 2000 to 2500 mg taurine per kilogram dry weight are thought to maintain normal plasma taurine concentrations in adult cats. It is also recommended that re-evaluation of plasma taurine concentrations be recommended 2-4 weeks after discontinuation of the drug. DCM due to taurine deficiency in cats that survive one month after initial diagnosis can often be weaned off all or most medications except taurine. These cats are known to have a 50% chance of surviving 1 year. Prognosis for cats with DCM
, not related to taurine or those that do not respond to taurine therapy are very poor.
Thromboembolism in a cat with DCM is a serious and completely unfavorable sign. ^Top
Disease prognosis
The disease development scenario is determined by the following factors:
- timely detection of the disease;
- degree of severity of symptoms;
- the presence of swelling and thromboembolism.
If the pathology is detected at an early stage, subject to proper nutrition and well-chosen therapy, the prognosis is favorable. Life expectancy is not reduced. If left untreated, the pet dies. Death occurs due to thrombosis or heart failure.
Stress can make your pet's condition worse
It is important to remember that any stress can worsen a pet’s physical condition. Therefore, it is necessary to protect the animal from emotional stress.
Prognosis for a cat when the disease is detected
The forecast depends on the following factors:
- timely detection of pathology;
- manifestations of clinical signs;
- severity of symptoms;
- likelihood of pulmonary edema;
- presence of thromboembolism.
Veterinary practice shows that cats with moderate enlargement of the left ventricle and atrium often live to an advanced age. In the presence of severe heart failure and congestion, the prognosis is cautious. Cats with significant hypertrophy of the heart muscle live 1 - 3 years. The prognosis is even more cautious, even unfavorable, with the development of thromboembolism.
We recommend reading about cirrhosis in cats. You will learn about the causes of primary and secondary cirrhosis in a pet, symptoms, diagnosis, treatment, prognosis. And here is more information about the best methods of treating urolithiasis in cats.
Prevention of HCM
The leading preventive direction is early diagnosis. Your pet should be brought in regularly for examination using echocardiography. You should also enrich the animal’s diet with proteins and taurine.
Cats suffering from cardiomyopathy do not participate in breeding.
Timely diagnosis of the disease is the best preventive measure
Hypertrophic cardiomyopathy is a common pathology among cats. Maine Coons and Ragdolls are more susceptible to the disease. Therefore, owners of representatives of these breeds should be extremely attentive to the physical condition of the pet.
Interesting facts from the medical history
Hypertrophic cardiomyopathy is a relatively new disease in veterinary practice. Intensive research into cardiac pathology began in the early 2000s in the United States. A large population of Maine Coon and Ragdoll cats was scientifically analyzed for carriage of a mutation leading to heart disease.
American scientists have concluded that a mutation in the gene responsible for the myosin-binding protein is the main cause of the genetic predisposition of Maine Coons and Ragdoll cats to hypertrophic cardiomyopathy.
Based on the research conducted, genetic test systems were created. However, their widespread use was not justified, since even with the selection of mutation-negative sires, cases of heart disease were encountered in the offspring.
By 2010, German scientists had completed large-scale studies of a large population of Maine Coons and Ragdolls in order to identify carriers of the mutation. It turned out that the genetic tests proposed by American scientists and widely used throughout the world are reliable only for cat populations in the United States.
We recommend reading about heart disease in cats. You will learn about congenital and acquired heart diseases, symptoms that should alert the owner, diagnosis and treatment. And here is more information about the causes and treatment of endometritis in cats.
Treatment for a pet who has had a heart attack
The very first thing that the owner of a cat who has suffered a heart attack must understand is that the treatment must be completely carried out by a veterinarian. It is unacceptable to try to treat an animal yourself, especially with drugs that are intended for humans. Be sure to follow the medication regimen prescribed by your doctor. Do not change the dosage or rely on the opinions of people whose animals have experienced something similar. It is important to realize that each case is individual.
The beginning of therapy involves taking a drug such as Nitroglycerin or its closest analogues. In addition, the specialist also prescribes anticoagulants that prevent the animal from developing blood clots. The veterinarian must prescribe a diet suitable for the cat’s condition. It should consist of food that is easily digested and absorbed by the stomach. Of animal proteins, it is permissible to include only fermented milk products in the diet, but not particularly fatty ones.
A cat who has had a heart attack is given a saline drip to avoid dehydration. In conjunction with this, injectable solutions of saline and glucose are also recommended, which are administered one at a time. Of the medications in tablets, the doctor prescribes to the patient those that have a mild sedative effect and are able to support a depleted heart.
Rest is the key to a quick recovery for a mustachioed friend who has suffered a myocardial infarction. The owner must protect it from excessive loads and noise. If there are children in the family, then you need to ask them not to play with the animal for a while and not disturb it without doing anything. Failure to follow these simple recommendations can contribute to a rapid relapse of the disease. The chances of surviving a second heart attack for any individual are zero.
Due to the fact that necrosis of the myocardium has already occurred, one should not hope for an absolute recovery. A scar formed on the heart muscle will prevent its normal contraction. Remember that the health of the nervous system and the absence of shocks will help the cat live a long and fulfilling life.
What is fainting
Loss of consciousness due to insufficient blood circulation in the vessels of the brain is fainting. A characteristic feature of the condition is its short duration.
Types of fainting
Loss of consciousness can be of different nature:
- non-epileptic;
- epileptic.
The first condition is caused by a diffuse metabolic disorder of brain tissue, which is usually triggered by a transient decrease in blood flow through the arteries of the brain.
Epileptic syncope is of a completely different nature, and its treatment differs from that of non-epileptic loss of consciousness.
Stages and warning signs of syncope
The general condition clinic consists of several stages:
- Harbingers.
- The period of being unconscious.
- Recovery stage
A cat, unfortunately, cannot complain about general malaise, lightheadedness, or “flies” flashing before its eyes. But an attentive owner can detect changes in the pet’s condition. Especially if syncope recurs.
Signs of fainting in a cat
At the warning stage, the clinical picture of fainting boils down to lack of air and dizziness. In a cat, these conditions manifest themselves as:
- severe weakness, unsteadiness when walking;
- coordination violations;
- vocalizations (the cat screams before syncope);
- vomiting;
- absent look;
- cold extremities;
- pallor of visible mucous membranes and skin (but in a cat this sign is almost impossible to notice).
Then comes the actual stage of loss of consciousness. During this period, there may be involuntary acts of urination or defecation. The animal's paws are extended forward and its head is thrown back. These same signs are characteristic of epileptic seizures. Conditions associated with epileptic activity and those not associated with it must be differentiated, since the treatment in these cases will be completely different. Therefore, if the owner has the opportunity to record a video of his pet fainting, it is better to do this in order to show it to the doctor.
Next comes the recovery period. During this period, some weakness, dizziness, and low blood pressure persist. In some cases, the animal behaves after fainting as if nothing had happened.
Caring for a sick animal
In the period after acute symptoms have resolved, your pet should be provided with special care that will help it live several more happy years.
New way of life
The main condition for recovery is complete rest. You can’t tug at your mustachioed friend again or allow him to jump from a height. It is worth limiting visits to public places. While walking, you should not go to parks with large concentrations of other animals that could chase or scare your recovering pet. It is better to refrain from walking altogether for a long time.
Stressful situations should be minimized. Do not allow rapid heartbeat.
The room where the patient lives must be well ventilated. However, it is unacceptable to allow the cat to be in drafts. Your pet should have a dark corner where he can hide from everyone.
What to feed your pet
Much attention in the post-infarction period is paid to nutrition. Now the menu should consist of easily digestible foods: carbohydrate foods, fermented milk products, fatty protein foods are excluded. Porridge can be cooked not only in water, but also in low-fat chicken broth.
Be sure to exclude lard, fish, smoked, fried and salted foods from the diet. You should not give your recovering friend food from your host’s table. It contains a large amount of seasonings and preservatives, which are bad for your health. But a diet of meat and vegetables is good for your pet.
If your pet is accustomed to eating ready-made industrial food, then you need to pay attention to its composition. They shouldn't be of poor quality. A recovering cat should be switched to premium food or higher, which can be purchased at veterinary pharmacies. In addition to nutrients, they contain elements and vitamins that are beneficial for the cardiovascular system. The names of the foods will be recommended by the treating veterinarian.