Dermatophytosis in cats - what is it?
All fungal infections are united under one name - dermatophytosis. This disease can affect not only animals, but also people. Develops on hair (fur), claws. In some forms, the spores accumulate in the inner and outer layers of the skin. The infection is caused by fungi of the species Microsporum gypseum, Microsporum canis, and less commonly Trichophyton. Unfortunately, any animal can become infected with them. The disease is common among felines. It has been noted that it can go away on its own without treatment, but then the individual becomes a passive carrier. Animals with weak immunity have difficulty coping with infection. It is fraught with complications and even death.
The danger of this disease is that it is transmitted. Not only other animals, but also owners are at risk. Therefore, it is extremely important to know how the infection manifests itself, how it is transmitted and how it is treated.
Causes
Cats are usually affected by the fungus Microsporum canis, and less commonly by Trychophyton mentagrophytes. A pet can become infected in various ways:
- from a sick animal (not only from other cats, but also from dogs or rodents) with fur, skin flakes;
- through an infected environment (fungal spores are extremely resistant to disinfectants and can remain viable for 1.5 years);
- with care items (comb, bedding, scratching post).
The body is able to protect itself from fungal infection at the cellular level, so an adult healthy animal does not always become infected with dermatophytosis, even when in contact with sick relatives. Various factors weaken the immune system and protective properties of the skin:
- young age (immunity is not yet fully formed) – kittens are most susceptible to infection;
- viral diseases (including immunodeficiency and feline leukemia);
- tumor processes in the body;
- inadequate, unbalanced feeding;
- treatment with anti-inflammatory drugs or other drugs that suppress the immune system;
- pregnancy and lactation;
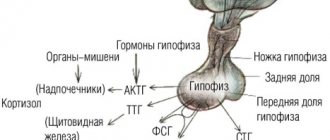
- systemic diseases - diabetes mellitus, Cushing's syndrome;
- stress.
Any skin disease accompanied by scratching, such as flea infestation or subcutaneous mites, can trigger the development of dermatophytosis. It is easier for fungal spores to penetrate the skin in damaged areas.
The time from infection to the appearance of clinical signs is 1-3 weeks. Fungi attack the skin and growing hair. Cats get shingles much less often than dogs because they actively groom themselves. During grooming, they remove fungal spores from their fur.
Signs
Dermatophytosis in cats can manifest itself in different ways. Everything will depend on the general condition of the body and immunity. In most cases, the affected area on the animal's body becomes bald. Scaly gray crusts may form on the skin.
Most often, fungal infection is localized on the paws, face and ears. The disease does not manifest itself as severe itching, it may be absent altogether, so special treatment is not required to combat the symptoms.
Signs of dermatophytosis in cats may be different. The disease manifests itself in the following forms:
- Extensive damage to the skin. There is peeling and a change in color to red.
- Quite deep inflammation of the dermis. A local type of furunculosis occurs.
- Formation of acne (comedones).
- Inflammation of the hair follicles on the chin.
- Formation of crusts on the skin (diffuse alopecia).
- Increased production of sebaceous gland secretion.
- Dermatitis with large lesions.
It is worth noting that the fungus can “settle” not only on the body, but also on the claws. This form of the disease is called onychomycosis. Rarely diagnosed. In some cases, doctors resort to removing the damaged phalanx.
Individuals of the Persian breed are susceptible to pseudomycetoma. A fungal disease of this form occurs in the form of a dense subcutaneous formation. This is where pathogenic microorganisms develop. They penetrate into the inner layers through destroyed follicles. This can lead to the formation of fistulas. When pseudomycetoma is removed, there is a high probability of relapse if the animal has not completed a course of antifungal therapy.
Dermatomycosis and its pathogens
The main manifestation of dermatomycosis is the appearance on the animal’s skin of lesions with sparse hair or no hair at all. With this disease, the epidermis, hair shaft and the skin itself are affected.
The photo shows the causative agent of dermatomycosis, magnified under a microscope.
The most common is:
- infection caused by 2 pathogens: trichophytosis and microsporia;
- Cats of any age can become infected, young animals are especially susceptible;
- transmission of the disease occurs at any time of the year;
- the incubation period is 5-40 days, depending on the animal’s immune system.
The disease is caused by spores of imperfect dermatophyte fungi that feed on the horny derivatives of the epidermis of the skin.
Dermatophyte pathogens are divided into several groups:
- The habitat of geophiles is the ground, infection occurs after contact with the soil;
- carriers of zoophilic pathogens are animals, they are transmitted under the condition of similarity of keratin;
- Anthropophilic diseases infect people from each other; the disease can be epidemic in nature.
Classification occurs depending on the type of tissue affected:
- with epidermophytosis, the stratum corneum of the epidermis suffers;
- disturbances in the stratum corneum of the epidermis and hairline are caused by trichophytosis;
- onychomycosis affects the horny mass of the nails.
A cat becomes infected during contact with another animal or at the moment of contact with inseminated objects or soil.
Diagnostics
In order to diagnose dermatophytosis in cats in a timely manner, it is recommended to do fungal tests for any damage to the skin. To do this, you need to visit a specialized clinic. At the appointment, the doctor will examine the damage and assess the condition of the entire skin. A rapid test is also required to determine the presence of parasites. After this, you need to check whether there is a fungal infection on the animal’s fur. To do this, you will need to turn off the lights in the office or go into a dark room and use ultraviolet light to examine the cat’s body, paws, head, and tail. Areas containing fungal spores glow yellow-green, and quite brightly. However, if the lesion is caused by Microsporum canis, then this method is effective only in 50% of cases. The fact is that this type of fungus may not fluoresce.
It is important to know some points:
- If the owner of the animal has already started treating the fur with preparations (ointments, creams, lotions), then there will be no reaction to ultraviolet radiation.
- When working with a Wood's lamp, you must take into account that if you do not warm it up, there is a high probability of obtaining a false result.
The glow method, although it has disadvantages, is widely used. It's pretty simple. Cats tolerate such diagnostics calmly. The only thing is that using ultraviolet light can only make a preliminary diagnosis. To confirm it, you will need a wool study. To do this, the doctor pulls out several hairs. Places them in mineral oil and conducts a microscopic examination. This allows you to determine the presence of spores.
However, in medicine, bacterial culture is considered the most reliable analysis. To do this, particles are combed from the animal’s fur using a special stiff brush, which will become the material for research. Next, they are placed in a container and sown on a nutrient medium for some time. Thanks to this analysis, it is possible to establish not only the presence of a fungal infection, but also the type of microorganisms. And this, accordingly, will allow the doctor to choose effective treatment.
Treatment of ringworm in dogs
Treatment of dermatomycosis in dogs can be vaccination or medication. Both methods are effective. The choice of one or another method of treatment depends on the condition of the pet and whether it has contraindications to taking or intramuscularly administering certain drugs.
Vaccines are not only an effective means of combating this disease, but also a good preventative measure that helps prevent its occurrence in your pet. Among the drugs that help cope with fungal infections, the most popular and those that have the most rapid and effective effect are:
- . This yellowish-brown drug is administered to the animal intramuscularly twice. The first time - in one limb, the second time - in the other. The interval between the first and second administration of the vaccine is from 10 to 14 days. As for the dosage, it does not differ depending on the purpose of such intramuscular intervention - treatment or prevention. For dogs that weigh less than 5 kg, the dose of the drug is 0.5 ml, and for pets whose weight exceeds 5 kg - 1 ml.
- "Polivak-TM". The medicine has a light brown tint. When storing the drug, sediment accumulates in it, so before drawing it into a syringe, the ampoule must be shaken so that the sediment dissolves. If the vaccine is administered for the purpose of treating dermatomycosis, then this procedure must be repeated 3 times with an interval between each administration of 10-14 days. Dosage - 0.5-0.6 ml. If the purpose of using the drug is prevention, two injections should be given at the same interval. In this case, a single dose of the drug should be no more than 0.3 ml.
Important!
Such injections should not be given to pets with a high temperature.
- Microderm. On pharmacy shelves or in veterinary stores, this drug can be found in two forms: dry (in the form of a gray-yellow porous mass that requires separate manipulations so that it can be administered intramuscularly) and liquid (a solution ready for use). If you purchased the vaccine in dry form, it must be mixed with saline or distilled water in the following proportions: 1 ml of liquid per dose of the drug. Detailed instructions for use should be indicated on the packaging or prescribed by a veterinarian. To use the vaccine in liquid form, simply shake the bottle with the drug. Microderm is administered twice only if the pet’s symptoms of the disease have not disappeared within 10-14 days after the first use. The dosage depends on the age and weight of the animal - puppies are usually administered from 0.5 ml to 1 ml, and adult pets - from 1 to 2 ml.
Do not be afraid of the ball that may appear after the injection of one of the above vaccines at the injection site: it will resolve within a few days after the procedure.
Antibiotics
As a rule, treatment with help is prescribed if there are contraindications to administering vaccines to a dog. Recommended drugs in tablets for the treatment of dermatomycosis in animals:
- "Griseofulvin" (such tablets should be used with caution due to their toxicity);
- Nizoral/ketoconazole (have almost identical composition and the same active ingredient);
- Itraconazole
The duration of treatment with antibiotics and their dosage are prescribed by a veterinarian, depending on the symptoms and stage of development of the disease.
In the case of drug treatment, it is necessary to treat the skin externally with antifungal ointments (clotrimazole, ketoconazole, nystatin, etc.). It is also recommended to trim around the affected areas. If the dog has long hair and there are many places affected by the fungus on its body, paws and face, it is better to shave it completely.
Deep dermatomycosis also involves washing animals with special shampoos.
Quite often, to combat this disease, doctors prescribe a course of treatment (from 10 to 15 sessions) using a quartz lamp (UVR). Such procedures involve exposing damaged parts of the skin to a lamp and initially last about 30 seconds. With each subsequent session, the duration of the procedure increases and at the end it is 2 minutes.
Important!
During such procedures, protect your pet's eyes from exposure to lamp light.
In kennels or any other places where there is a large concentration of dogs, outbreaks of ringworm are not uncommon. To avoid unpleasant epidemics, you need to regularly treat the area with alkali and solutions of salicylic or carbolic acids, and disinfect the premises using quartz lamps.
It is better to vaccinate against dermatomycosis every year for animals that often come into contact with possible carriers of fungi. To increase the resistance of your pet’s immunity to diseases of this kind, it is necessary for him to regularly take vitamin complexes. It is better to have them prescribed by a doctor. Ringworm is not a particularly dangerous disease and certainly does not threaten your pet's life, however, it can become a huge problem if the affected dog infects all family members.
Therefore, it is important to contact your veterinarian and begin treatment for the disease immediately after you notice characteristic spots on your dog’s skin. But an even more effective method of avoiding the troubles associated with ringworm, both for you and your pet, is to prevent the disease.
Ringworm, or canine tinea, is a fungal infection that affects the surface layers of the skin, fur, and nails of animals. As a rule, it is caused by such species of fungi as Microsporum canis, Microsporum gypseum and Trichophyton mentagrophytes.
Dogs can become infected from other dogs, cats, rodents and even hedgehogs. Direct contact between animals is not always necessary; infection can even occur through care items (for example, through bedding, shared toys). The risk of getting sick is higher in young dogs, in animals during pregnancy and feeding, as well as in dogs with concomitant viral infections. Poor nutrition and long-term treatment with anti-inflammatory drugs and drugs that suppress the immune system also contribute to shingles. There is also a breed predisposition to lichen - Yorkshire terriers suffer from it more often. Dermatophytes reproduce especially well at high temperatures and high humidity. This disease is potentially dangerous for people, especially those with reduced immunity.
Before starting treatment
Before you begin treatment for dermatophytosis in cats, you will need to treat the habitat. We are talking about the room where the animal lives. It is important to understand that if an individual is already infected with a fungus, then its spores remain on all places and objects with which it has been in contact. Naturally, this will reduce the effectiveness of treatment. Therefore, it is recommended to do the following:
- Clean the entire living space daily using a vacuum cleaner. Particular attention is paid to those places where the pet likes to spend time.
- If possible, treat surfaces with chlorine-based disinfectants.
- If two or more cats (or other animals) live in one room, then it is advisable to carry out disinfection using special antifungal sprays.
What should owners do?
With the help of relatively simple techniques, you can significantly speed up the healing process and significantly alleviate your pet’s condition. Here's what you can do for your dog:
- Apply miconazole-based ointments to the affected areas of the skin (in consultation with your veterinarian, of course).
- Wash your dog using shampoos with antifungal compounds. Again, their use should only be done with the knowledge and approval of a veterinarian.
- Preparations based on sulfur have also proven themselves well in treatment, so do not miss the chance to anoint bald areas of the skin with ordinary sulfur ointment.
You need to be prepared not only for the fact that you will have a devoted friend and protector, but also for caring for your pet and the difficulties that all dog owners face. One of these difficulties is pet illness.
It is very important to monitor the health and behavior of your pet, because he himself will not tell you what is bothering him, and there are enough dog diseases, as well as places where your dog can become infected with them. One of the common infections is dermatomycosis
, which is dangerous not only for the dog, but also for the owner, and therefore requires thoughtful treatment.
Local treatment
Most often, dermatophytosis in cats is treated at home using ointments, lotions, and creams. However, owners are still advised to contact a veterinary clinic to select effective antifungal therapy.
Before starting treatment, it is important to trim the animal's fur. Only after this is processing carried out. For it they use:
- Preparations with clotrimazole and miconazole in the form of creams or lotions. The affected areas are treated twice a day. When applying the drug, be sure to cover a larger area - expand its boundaries by 1-2 cm.
- Medicinal shampoo. It should contain antifungal agents (enilconazole, miconazole). There are also shampoos with the addition of chlorhexidine (4%). Used for extensive lesions. Use shampoo no more than twice a week.
Systemic therapy
As a rule, dermatophytosis in cats is treated with topical medications within three weeks. If therapy does not produce results, then the doctor decides to prescribe a systemic course. It has side effects, so you need to be treated under the supervision of a specialist, taking regular blood tests. This is necessary in order to track the number of white blood cells.
The duration of the course of taking systemic drugs is one and a half to two months. It may include Itraconazole or Griseofulvin. The first is prescribed in an amount of 10-20 mg. Take it either every other day or daily. The dosage of the second drug is 25-60 mg/kg. Cats are given it 1-2 times a day. Itraconazole is considered less toxic. It is more easily tolerated by animals and rarely causes side effects.
These drugs can disrupt development, so they should not be prescribed to kittens under three months old and to individuals who are expected to give birth.
If the fungal infection has spread to the claws, then Flucostat, Fluconazole, and Diflucan are prescribed. These drugs are quite effective. Dosage – 20-30 mg once a day.
About mushrooms
Fungi are ubiquitous in our environment.
Of the thousands of different species of fungi, only a few have the ability to cause disease in animals. The vast majority of fungi are either soil organisms or plant pathogens. However, more than 300 species of fungi have been described that can be pathogens. There are five kingdoms in nature: Monera (bacteria and blue-green algae), Protista (protozoa), Fungus (fungi), Plantae (plants), and Animalia (animals). Fungi are eukaryotes, do not contain chlorophyll, and can grow as yeasts (single-celled organisms), molds (multicellular fibrous organisms), or a mixed growth pattern. Fungal cell walls are composed of chitin, chitosan, glucan and mannan. The Fungal Kingdom includes five subkingdoms: Chytridiomycota, Zygomycota, Basidiomycota, Ascomycota, and Fungi Imperfecti or Deuteromycota. Special terms are used to refer to different parts of mushrooms:
- A hypha is a filamentous formation of fungi consisting of many cells.
- Mycelium is a set of hyphae.
- Septa are divisions between cells within hyphae.
- Conidia are non-motile spores of asexual reproduction in fungi (types of conidia: blastoconidia, arthroconidia, anneloconidia, fialoconidia, poroconidia and aluriconidia).
- Conidiophore is the mycelium on which conidia are located.
It is assumed that the hair growth phase is important for the development of infection. Hair infection begins and continues during the anagen phase. Spontaneous healing may occur during the telogen phase. It is also believed that self-healing may occur due to the development of an inflammatory reaction. It is in this regard that dermatophytosis is considered a self-healing disease. However, arthrospores can remain on the hair shaft, but re-infection of this particular hair follicle will occur only after the anagen phase begins again.
Epizootological data. When at an appointment we see a cat or dog that may have microsporia suspected, it is important to find out whether the animal had prior contact at exhibitions, or whether it was in foster care, for example, while the owners were on vacation. If an animal is selected or comes to us from a shelter or nursery, then the suspicion of a possible disease increases.
LUM diagnostics. The luminescent glow of affected hairs using a Wood's lamp allows them to be targeted for direct microscopy and culture. But, unfortunately, this method is reliable only in 50% of cases (photo 2, 3).
Recently, commercial veterinary tubes containing DTM media have become available on the market. This is a selective medium, the change in color from yellowish to red during the growth of dermatophytes can suggest the presence of infection. A definitive diagnosis can only be made by microscopy of the colony when characteristic macroconidia are detected. The advantage of this medium is that we see its red color, since growing dermatophytes, first feeding on the proteins in the medium, change its pH. It is important not to miss this moment, which occurs when we see the beginning of the growth of the colony. However, it must be remembered that other mushrooms can also change the color of the environment, thereby misleading us (photo 6). In our practice, there was a precedent when the DTM medium changed its color due to the growth of the Aspergillus fungus contaminating the skin. It is microscopy of the colony that is the main diagnostic aspect, allowing one to see macroconidia. But placing adhesive tape for a colony imprint in a jar with a small lid (that’s how DTM medium is sold) is quite a difficult task. Finally, DTM is several times more expensive than Sabouraud's medium. It is the latter medium, which does not contain indicators, that we prefer in our practice for growing dermatophyte colonies.
Ketoconazole is an antifungal imidazole. Action: antifungal. It disrupts the synthesis of ergosterol in the walls of fungal cells by inhibiting 14-α-demethylase, which belongs to the cytochrome P450 system. Inhibits the absorption of purine and disrupts the biosynthesis of triglycerides and phospholipids. Pharmacokinetics: absorption is enhanced when administered with fats and small amounts of food. High concentrations are achieved in the liver, kidneys, pituitary gland and adrenal glands. It is excreted in urine, sweat, sebum, earwax, saliva and milk. Metabolized in the liver to inactive metabolites, which are excreted in bile and feces. 10 to 14 days of treatment may be required (until steady-state levels and effective therapeutic concentrations are achieved in the skin). Indications: antifungal agent (canine dermatophytosis, Malassezia dermatitis, localized or disseminated candidiasis, blastomycosis, histoplasmosis, coccidioidomycosis and cryptococcosis). Not recommended for use in the treatment of feline dermatophytosis (preferably griseofulvin, itraconazole or fluconazole). At the same time, it was used with cyclosporine to reduce the rate of elimination and reduce the required dose of cyclosporine, which reduces the cost of treatment. It is not a first choice drug for animals with diseases of the central nervous system or eyes. Contraindications: pregnancy, lactation, liver dysfunction, thrombocytopenia. The drug should be used with caution or not at all when taking medications metabolized by P450 enzymes. Avoid use with mitotane, rifampin, and theophylline. Dosage: dogs: dermatophytosis – 10 mg/kg every 24 hours; cats: not recommended for use due to high incidence of side effects (loss of appetite, weight loss, hepatotoxicity). Side effects: anorexia, vomiting, diarrhea, weight loss, fever, depression, hepatotoxicity (hepatocellular necrosis), thrombocytopenia, non-regenerative anemia, teratogenic effect, decreased synthesis of cortisol and testosterone in dogs, decreased libido, gynecomastia, azoospermia, impotence, anestrus, itching , hair loss, lightening of the coat associated with loss of guard hairs, as well as cataracts after long-term therapy in dogs. Monitoring: Serum levels of liver enzymes (alanine aminotransferase, alkaline phosphatase), bilirubin, and bile acids should be assessed before treatment and during therapy (every 2–4 weeks).
Itraconazole is a synthetic triazole antifungal drug. Action: inhibits 14-α-demethylase, belonging to the cytochrome P450 system, preventing the synthesis of ergosterol in the cell membrane of the fungus, weakly binds to mammalian P450. Pharmacokinetics: Bioavailability is (approximately) 40% in the fasted state, increased when administered with food and acidic pH in the stomach. Penetrates poorly into the central nervous system or eye tissue. Metabolized in the liver into inactive metabolites, which are excreted in bile and urine. Indications: dermatophytes, Malassezia, candidiasis, blastomycosis, histoplasmosis, aspergillosis (low effectiveness against the nasal form), cryptococcosis, sporotrichosis, zygomycosis, chromomycosis, onychomycosis, as well as the protozoa Leishmania and Trypanosoma. Compared to ketoconazole, it has increased potency, reduced toxicity and a wider spectrum of action. Contraindications: liver disease or liver failure. Prolongs the effects and increases the toxicity of benzodiazepines (midazolam), cyclosporine, glucocorticoids, antihistamines, quinidine, digoxin, vincristine, warfarin, sulfonylurease. Contraindicated concomitantly with antacids, H2-blockers and anticholinergics. Dosage: Dogs: 5–10 mg/kg every 12–24 hours; cats: 5 mg/kg every 12 hours or 10 mg/kg every 24 hours. For cats and small dogs, capsules can be opened and granules mixed with food. The dosage can be reduced by 25–50% when using the oral suspension without food. Pulse dosing regimens can be used in the treatment of superficial fungal infections. Thus, in the treatment of dermatophytosis, a dosage of 5 mg/kg was used for 7 days every other week, then repeating this therapeutic course at intervals every other week. Side effects: vomiting, diarrhea, abdominal pain, loss of appetite, increased serum liver enzymes, increased serum urea nitrogen, fever, increased blood pressure, skin rash, peripheral edema and ulcers due to cutaneous vasculitis (most common in dogs receiving more than 10 mg/kg/day twice daily). May be teratogenic and should not be given to pregnant or lactating animals. Monitoring: Liver enzyme levels should be monitored every 2 weeks and the medication should be discontinued if any side effects develop. You can try starting treatment again at a 50% dose reduction after the side effects disappear.
Action: antifungal, inhibits the synthesis of sterol and cytochrome P450. Higher affinity for fungal enzymes than ketoconazole and itraconazole. Pharmacokinetics: high bioavailability (> 90%), absorption in the gastrointestinal tract is not affected by food intake and changes in pH in the stomach. Penetrates well into the central nervous system and eye tissue, regardless of the presence of inflammation. Indications: excellent drug against yeast, including Cryptococcus, Blastomyces, Histoplasma, Coccidioides, Malassezia, Candida; has variable activity against filamentous fungi such as Aspergillus and dermatophytes. Contraindications: dosage is reduced in case of renal failure; use of the drug in pregnant animals should be avoided. Cimetidine may interfere with absorption. Enhances the activity of anticoagulants, thiazide diuretics, rifampin, cyclosporine, glipizide, antihistamines, diphenylhydantoin and theophylline. Dosage: Dogs: 2.5–5 mg/kg every 12–24 hours; cats: 5–10 mg/kg every 12–24 hours. Side effects: vomiting, diarrhea, abdominal discomfort, skin rash, hepatotoxicity (less common than with ketoconazole and itraconazole). Does not suppress adrenal hormones or sex hormones. Monitoring: liver enzyme levels are assessed before and (monthly) during treatment. Additional information: In one in vitro study of 30 M. canis isolates, all 30 were found to be resistant to fluconazole.
Terbinafine is an allylamine. Action: inhibits the biosynthesis of ergosterol and squalene epoxidase, which leads to ergosterol deficiency in the cell wall of the fungus and intracellular accumulation of squalene. Terbinafine has fungistatic and fungicidal effects because it is not primarily an inhibitor of cytochrome P450 systems. It is more selective than azoles. Pharmacokinetics: absorption is enhanced when administered with fatty foods. Highly lipophilic and keratinophilic. Found in high concentrations in sweat, sebum, skin, nail beds and fur. Metabolized by the liver and excreted in the urine. Local drugs have minimal absorption (
Many people, when getting a kitten, are not even aware of the difficulties they may encounter. Unfortunately, the pet not only plays, but also gets sick. Fungal infections are the most common. Let's figure out what dermatophytosis is and how to deal with it.
"Vacderm-F"
Vaccines are used as a preventive measure, as well as a treatment for dermatophytosis in cats. The products are considered universal because they have a wide spectrum of action. If the animal has not been vaccinated, it is recommended to use the Vakderm-F vaccine for treatment. It is designed specifically for cats and is most effective in combating fungal infections.
Duration of treatment
Having decided what and how to treat dermatophytosis in a cat, it is necessary to say a few words about the duration of therapeutic courses. It is important to remember that this should be monitored by a qualified doctor. It is he who prescribes medications, determining the duration of their use. Afterwards you will need to do tests for the presence of pathogens. If the result is negative, then the course is repeated at seven-day intervals. Then another sample is taken. And if it is also negative, then you can finish the treatment.
In a situation where the tests raise doubts among the veterinarian, therapy continues. The recovery of a pet can be judged only after receiving at least two negative samples.
ethnoscience
Some owners use herbal medicine to combat dermatophytosis in cats. When treating at home, it is recommended to use a collection of herbs. It should include:
- birch leaves;
- St. John's wort;
- sagebrush;
- medicinal marigolds;
- Oak bark;
- marsh cudweed;
- meadow clover;
- tansy (inflorescences);
- yarrow;
- dried sage leaf;
- chamomile (flowers);
- burdock leaves.
An infusion is prepared from this herbal collection. To do this, pour boiling water over the mixture. Dosage – 0.5 l per tablespoon. The maximum infusion time for the decoction is 3 days. For prevention, the animal is given 4-5 ml before feeding 30 minutes. Sick individuals take 8-10 ml 2-3 times a day.
If this pathology causes ulcers or wounds to form on the cat’s body, then you can use calendula infusion. It promotes rapid healing.
Symptoms of ringworm
During the incubation period, humans can infect cats.
Dermatophytosis is an extremely contagious disease that can be transmitted from one animal to another, and then to humans. The infection can persist in the pet’s body for up to 6 years and not reveal itself in any way. During the incubation period (8-22 days), the fungus actively develops and spreads, although symptoms of the disease do not appear. Therefore, the animal is capable of infecting people and other pets.
As the disease progresses, cats' fur becomes brittle and round bald patches form. They are localized in the head area (on the ears, crown) and at the tip of the tail. Sphynx cats develop red sores on their bodies. At first these may be small foci of the disease, which later merge into one spot. Bald spots are not always noticeable in long-haired breeds, as they are hidden behind the hair. The skin takes on a grayish tint and begins to peel off. The affected areas are itchy and cause discomfort to the cat. Suppurations appear, which later become scars. Without treatment, dermatophytosis can lead to inflammation of the hair follicles.
Danger to humans
Dermatophytosis in cats (in the photo you can see what sick animals look like) is not so harmless. The disease poses a danger not only to other individuals, but also to humans. The fungus can enter through wounds and abrasions on the skin. At risk are people with weakened immune systems, children and the elderly.
If the animal is sick, the owner will have to limit not only contact with it, but also the pet’s movement around the rooms. It is better to handle a cat with gloves. It is also very important to perform proper hygiene procedures. Be sure to wash your hands thoroughly with soap and shower. In addition, it is necessary to clean and treat surfaces with special disinfectants. Using a steam generator is effective in combating fungus.
Are there risks of human infection from a cat?
Ringworm can be transmitted quite easily to people, especially children. This is why it is important to take appropriate steps to minimize exposure to fungus while treating your cat (see above: disinfecting the apartment and environment). Ringworm is most likely to be transmitted and cause clinical signs in people with suppressed immune systems.
If anyone in the home develops skin lesions, especially small patches of thickened or red skin with raised, scaly edges, medical attention should be sought. Ringworm in humans is generally very treatable. However, ringworm spores can remain infectious for up to 18 months in the environment. Consequently, re-infection may occur. When handling infected animals, it is important to wear gloves and wash your hands thoroughly afterwards.